Modality
Mammography
Introduction
A mammogram is a low dose x-ray examination of the breast that is used to screen for breast cancer. Mammography has been proven to decrease deaths from breast cancer and mitigate suffering from breast cancer and breast cancer treatments. Screening mammography finds the majority of cancers before they are felt by the patient or provider. Screening mammography is able to depict breast cancer at an earlier stage – often before it has spread outside the breast.
Mammography is also used in the diagnostic setting to further characterize an abnormality found during screening or to evaluate a patient or provider’s concern about a physical examination sign or symptom. Breast ultrasound, MRI and image guided minimally invasive core biopsies are frequently performed to diagnose breast abnormalities. Screening mammography is a standardized program with federal law (The Mammography Quality Standards Act) governing the equipment, procedures and personnel. Outcome auditing is performed regularly to assess program quality.
How Images Are Obtained

The mammographic unit is shown on the right. The breast is compressed between a plastic plate and the X-ray detector. This compression improves the visibility of normal and abnormal structures within the breast, decreases x-ray dose and reduces patient motion during the exposure.
The gantry can rotate 360 degrees, depending on the view desired. In the position shown, it will take a cranio-caudal "CC" view.
Two standard views are obtained of each breast in a screening mammogram, the cranio-caudal "CC" view and the medio-lateral oblique view "MLO" view.
Cranio-Caudal View - the breast is compressed from top to bottom. The x-ray photons pass through the breast from the head to the feet and are registered at the detector below the breast.
Medial Lateral Oblique View - utilizing the obliquity of the pectoralis major as the axis for positioning the gantry holding the compression plate and detector, the breast is compressed obliquely, and the photons pass through the breast and are registered at the detector below. The green dot indicates the axillary tail of the breast.


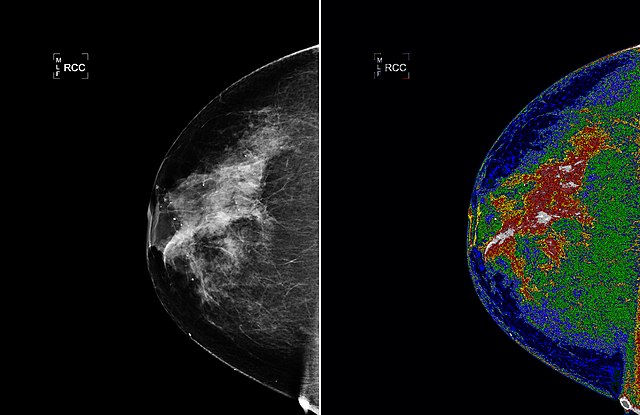
Cranio-Caudal View
The x-ray photons pass through the breast from superior to inferior and are registered at the detector below the breast.
The images are viewed back to back to compare the fibroglandular tissue in each breast and optimize detection of asymmetries.
By convention the laterality markers (RCC, LCC) are always placed at the lateral aspect of the breast.
Identify the following structures:
- Medial Breast
- Lateral Breast

Medial Lateral Oblique View
Utilizing the obliquity of the pectoralis major as the axis for positioning the gantry holding the compression plate and detector, the breast is compressed obliquely, from axilla to the lower inner breast. The x-ray beam passes through the breast from medial to lateral.
The images are viewed back to back to compare the fibroglandular tissue and optimize detection of asymmetries. The axilla is at the top of the image and the inferior breast at the bottom.
Identify the following structures:
- Pectoralis Major Muscle

Additional Views
Different views and techniques can be done to problem solve. Some examples include:
- Magnification views – Increasing the distance from the breast to the receptor plate allows magnification and increased spatial resolution and thereby helps characterize the size and shape of calcium particles and margins of masses. The image on the left is a standard CC view and on the right a coned down, magnified view of the area of concern. The green circle highlights the mass.

Magnification View of Suspicious Mass - Lateral-medial (“LM”) view – The beam passes lateral to medial. This view helps depict a lesion in a true orthogonal view to facilitate directed ultrasound or core biopsy. It is also helpful in characterizing benign “milk of calcium” which layers when viewed from the side.
- Spot Compression – These views use a small paddle to provide focal additional compression, to improve conspicuity of a specific area of interest.
- Rolled View – The top of the breast is rolled relative to the bottom to spread out the tissues and provide information about the presence and location of findings seen only seen in one plane.
- Exaggerated Lateral Cranial-caudal view (
XCCL) – Used to better evaluate lateral tissue in the cranio-caudal projection. - Cleavage View – Optimizes inclusion of medial tissues in the cranio-caudal view through including
Factors Affecting Appearance
Breast Density
The composition of the breast affects the appearance of the image and the sensitivity of the study for detection of abnormal soft tissue densities. Radiologists are required to report the breast composition in their reports to alert the reader to the relative sensitivity of the study for detection of non-calcified cancers. There are four categories of breast density.
- Fatty
- Scattered
- Heterogeneously dense
- Extremely dense
The image below depicts the two extremes of breast composition.
Identify the following structures:
- Fatty Breast (Left)
- Extremely Dense Breast (Right)

Importance of breast compression
Compression of the breast between the plate and the detector spreads out the overlapping breast tissues. Degree of compression is measured in Lbs.
Compression helps to differentiate true masses from summation shadows that occur because of overlapping soft tissues. Compression renders the breast nearly uniform in thickness so the film density of tissues near the nipple will be similar to those near the chest wall. This also decreases the radiation dose to the breast.
Note that in this image, 33 Lbs of compression results in less overlap and improved conspicuity of the fibroglandular tissues compared with 17 Lbs.

What to look for
The normal features of the breast are scrutinized when interpreting a mammogram. The images below demonstrate normal anatomy on 'CC' and 'MLO' views.
Identify the following structures:
- Nipple
- Subcutaneous Fat
- Fibroglandular Tissue
- Retroglandular Fat
- Medial
- Lateral
- Cooper's Ligaments

Masses
Breast cancer can have several different appearances on mammography. The next few images demonstrate the most common mammographic findings of breast cancer.
The most specific sign of malignancy on mammography is a lobulated (bumpy) spiculated mass. Spiculations describe the linear strands/spikes extending outward from the mass, like spokes on a wheel.
The green circle on this image highlights a spiculated mass that is highly suspicious for cancer. This is a magnified view taken after a suspicious area was identified on the screening mammogram.

Architectural distortion
Architectural distortion is perceived as straightened lines or lines converging on a central point. This pattern is atypical for normal fibroglandular tissue, but is seen with breast carcinomas.
This image shows a standard and magnified view with the yellow box highlighting an area of architectural distortion.

Microcalcifications
Calcifications are fairly common within the breast and are usually benign, caused by things like arterial atherosclerosis and fat necrosis.
Specific patterns of microcalcifications can be seen with carcinomas, which can be detected on mammography. Pleomorphic (irregular shapes and sizes) groups (clusters) are a sign of cancer.
This magnified view demonstrates a cluster of irregularly shaped pleomorphic calcifications.

New Technology
Digital Mammography
Until 2000 the detector was a piece of film in a cassette. This was known as “film screen” mammography. Among other disadvantages, film was a medium that could not be shared and could be lost or damaged.
In 2000 the FDA approved “digital mammography” systems. The detector is no longer a piece of film, rather a photon receptor that converts the photons to a digital signal that can be viewed on a high resolution monitor instead of a lightbox. Digital mammography has largely replaced film based screening. As of 2015, 95% of all units in the United States are full field digital units.
This image shows the differing conspicuity of breast tissue on film screen vs digital mammography.

3D Tomosynthesis
Also called “3-D Mammography”, 3D tomosynthesis acquires a variable number of images in an arc-like swing of the camera and recreates the information into a series of 1 mm slices, the number of slices depending on the thickness of the compressed breast. This method reduces overlapping tissue superimposition, improving both sensitivity and specificity.
As of 2016, the technology has gained wide acceptance because of the ability to detect 40% more invasive cancers and avert 20% of recalls (recalls are additional images obtained to clarify otherwise normal structures). As of 2016 50% of sites had at least one 3-D tomosynthesis unit.
This image is a 1mm thick image from a tomosynthesis, showing an area of architectural distortion.

The images obtained with tomosynthesis can be viewed as a movie. Look for the area of architectural distortion as it comes into focus in the medial breast, about midway through the video.
Interpretation
Mammograms are considered one of the more difficult studies that radiologists interpret. Specific training is federally mandated to legally interpret mammograms for signs of cancer.
All projections should be labeled stating the view and breast being displayed. The radiologist should assess if there is adequate penetration and compression of tissue.
Factors to assess
- Is there adequate tissue included?
- Is the pectoralis major included in MLO view?
- Is the nipple in profile?
- Is the retroglandular fat included?

Breast cancer
When reading a mammogram, it’s best to have a search pattern to prevent misses. Compare one breast to the other, zone by zone. They tend to be fairly symmetric. It is also essential to compare each view against older mammograms, to find subtle changes over time.
Compare the CC view of the left breast from 2015 to the image from 2016. Do you see the area of breast tissue that has changed?

New findings 2016: Note the increased density and new pleomorphic calcifications. These are very suspicious for breast cancer.

